Credentialing & Privileging | 11.17.20
Understanding Reporting to the National Practitioner Data Bank for Communication and Resolution Programs
by Patricia Folcarelli, RN, MA, PhD; Lauge Sokol-Hessner, MD; and Melinda Van Niel, MBA, CPHRM
Communication and Resolution Programs (CRPs) have developed as a patient- and clinician-centered approach to resolving adverse events in healthcare settings. CRPs differ from traditional settlements or judgments in that they require the physician(s) involved to be honest and transparent about any adverse event that occurred, express empathy for the consequences of the event, and engage in improving systems of care in response to the root cause analysis following the event to prevent recurrence. The benefits of CRPs are numerous, including improved patient safety, more efficient resolution, and preservation or repair of the clinician-patient relationship.
As credentialing services staff are well aware, any payment made in response to a written claim on behalf of an individual physician must be reported to the National Practitioner Data Bank (NPDB). Although CRP resolutions may meet these criteria for a report, the traditional reporting options do not adequately acknowledge the efforts clinicians who participate in CRPs have made to respectfully, quickly, and fairly resolve the event for the patient and family. For this reason, the Massachusetts Alliance for Communication and Resolution (MACRMI) and the Collaborative for Accountability and Improvement (CAI) have been working with the NPDB to add an option to their reporting form to help clarify that a payment made to a patient through a CRP is not a settlement or award resulting from litigation.
As of June 2020, the NPDB has made changes to their reporting form in light of the prevalence of CRPs. On page 6, the “Payment Result of:” section now has an “Other” option, instead of the “Settlement Judgement or Payment Prior to Settlement” options which existed previously. Now, “Other” should be selected when a payment has been made on behalf of a physician through a CRP.

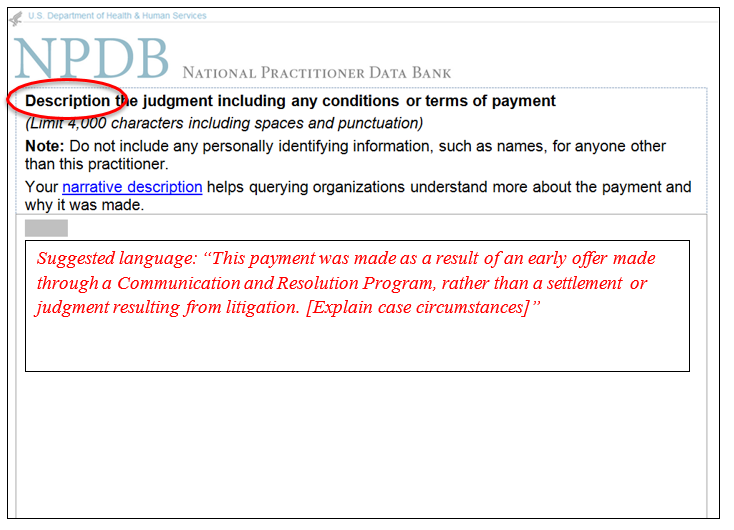
In addition, on page 7 of the NPDB report form, there is a new “Description” box to explain the conditions or terms of the payment. It is suggested that when describing a CRP payment in this box, language such as the following will help make the case resolution clear:
“This payment was made as a result of an early offer made through a Communication and Resolution Program, rather than a settlement or judgment resulting from litigation. [Explain case circumstances].”
Using this type of description and the “Other” option will help those using the NPDB when credentialing clinicians to better understand the nature of the payment and the proactive response of the clinician and healthcare facility to the adverse event. We encourage you to educate your medical staff services and risk management teams about these changes, as CRPs are becoming increasingly prevalent across the United States. Making use of these new options better acknowledges the patient-centered efforts of physicians who participate in CRPs after adverse events. In addition to ensuring that those involved in the physician hiring and credentialing processes have a more accurate and complete understanding of physicians’ malpractice records, this important development also may help CRP programs develop and spread, which may help drive improvements in the quality and safety of care.
 Patricia H. Folcarelli, RN, MA, PhD, is the vice president of patient safety at CRICO. Prior to joining CRICO, Pat was the vice president for health care quality at Beth Israel Deaconess Medical Center. Pat also is a lecturer on medicine at Harvard Medical School. Pat received her BS in nursing from Hunter College of the City University of New York, and an MA and PhD from New York University. Pat served on the board of the Massachusetts Coalition for the Prevention of Medical Errors and currently serves on the quality and safety board for Mercy, a health system in St. Louis and the Baystate Health Quality and Safety Board Subcommittee. Pat served as the board chair for Medically Induced Trauma Support Services (MITSS) and is the past president for Massachusetts Society for Healthcare Risk Management. Pat was involved in research activity focused on communication apology and resolution, workplace violence prevention, as well as work to eliminate the emotional harm from disrespect in healthcare.
Patricia H. Folcarelli, RN, MA, PhD, is the vice president of patient safety at CRICO. Prior to joining CRICO, Pat was the vice president for health care quality at Beth Israel Deaconess Medical Center. Pat also is a lecturer on medicine at Harvard Medical School. Pat received her BS in nursing from Hunter College of the City University of New York, and an MA and PhD from New York University. Pat served on the board of the Massachusetts Coalition for the Prevention of Medical Errors and currently serves on the quality and safety board for Mercy, a health system in St. Louis and the Baystate Health Quality and Safety Board Subcommittee. Pat served as the board chair for Medically Induced Trauma Support Services (MITSS) and is the past president for Massachusetts Society for Healthcare Risk Management. Pat was involved in research activity focused on communication apology and resolution, workplace violence prevention, as well as work to eliminate the emotional harm from disrespect in healthcare.
 Lauge Sokol-Hessner, MD, is a hospitalist and the medical director of patient safety in the department of health care quality at Beth Israel Deaconess Medical Center (BIDMC) in Boston. At Harvard Medical School, he is an assistant professor of medicine, the program director and BIDMC site director for the Harvard Medical School (HMS)/CRICO fellowship in quality and patient safety, and a course director for the HMS masters in healthcare quality and safety.
Lauge Sokol-Hessner, MD, is a hospitalist and the medical director of patient safety in the department of health care quality at Beth Israel Deaconess Medical Center (BIDMC) in Boston. At Harvard Medical School, he is an assistant professor of medicine, the program director and BIDMC site director for the Harvard Medical School (HMS)/CRICO fellowship in quality and patient safety, and a course director for the HMS masters in healthcare quality and safety.
 Melinda B. Van Niel, MBA, CPHRM, manages the Massachusetts Alliance for Communication and Resolution following Medical Injury (MACRMI) and leads its implementation team. She previously worked as the manager of patient safety at Beth Israel Deaconess Medical Center in the department health care quality, where she implemented one of the first Communication, Apology, and Resolution (CARe) programs in the state. She was a contributor and advisor to the AHRQ’s CANDOR Toolkit. Ms. Van Niel received her Bachelor of Arts degree from Harvard University and her Master of Business Administration from Villanova University with a concentration in healthcare management.
Melinda B. Van Niel, MBA, CPHRM, manages the Massachusetts Alliance for Communication and Resolution following Medical Injury (MACRMI) and leads its implementation team. She previously worked as the manager of patient safety at Beth Israel Deaconess Medical Center in the department health care quality, where she implemented one of the first Communication, Apology, and Resolution (CARe) programs in the state. She was a contributor and advisor to the AHRQ’s CANDOR Toolkit. Ms. Van Niel received her Bachelor of Arts degree from Harvard University and her Master of Business Administration from Villanova University with a concentration in healthcare management.